Knee Osteotomy
What is a Knee Osteotomy?
Knee osteotomy is a surgical procedure designed to shift the weight-bearing load from a damaged or arthritic part of the knee to a healthier area. This is done by cutting and reshaping the bones surrounding the knee joint.
Most osteotomies for knee arthritis are done on the tibia (shinbone) to correct a bowlegged alignment (varus) that puts too much stress on the knee's inner (medial) compartment. There are also osteotomies to correct excessive knock knees (vagus), and most of them are around the distal femur (thigh bone)
The procedure preserves the joint tissue rather than replace it, and this surgery can delay or prevent the need for a
Partial or
Total Knee Replacement.
Who is Suitable for Knee Osteotomy?
Knee osteotomy is typically recommended for young people (usually under 50 years old), active and have early-stage arthritis that only affects one part of the knee joint. Candidates for knee osteotomy should also have good knee alignment, be of average weight, and have no significant ligament damage.
What are the Benefits of Knee Osteotomy?
Knee osteotomy offers a range of benefits to patients, including
- Pain relief: Knee osteotomy can relieve pain caused by knee arthritis, allowing patients to resume activities they enjoy.
- Delayed need for knee replacement: Knee osteotomy can help delay the need for knee replacement surgery, a more invasive and complex procedure usually not ideal for young and active patients with higher demand.
- Improved function: Knee osteotomy can improve knee function, enabling patients to perform activities of daily living more comfortably.
- Quick recovery: Recovery from knee osteotomy is typically faster than knee replacement surgery, with most patients returning to normal activities within six months.
What are the Types of Knee Osteotomy?
There are several types of knee osteotomy, including
- High Tibial Osteotomy:
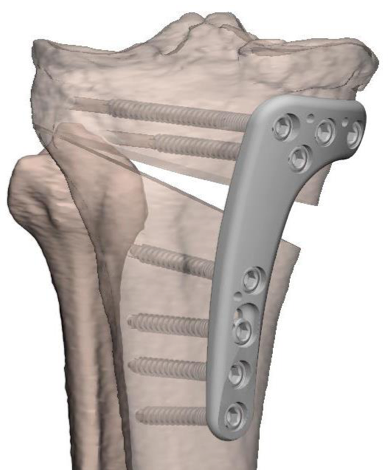
This is the most common type of knee osteotomy, which involves cutting and adding a bone wedge in the medial upper part of the shinbone to shift the weight-bearing load away from the damaged part of the knee. The surgeon employs Patient Specific Instruments to guarantee precision on cut and tailored accuracy to restore the patients' ideal alignment. A customised bone graft may or may not be needed, and a medial buttress plate and screws for fixation
- Distal Femoral Osteotomy: This is performed most of the time for patients with valgus (knock knees) alignment who have isolated lateral compartment wear. The procedure usually involves a precise cut in the distal femur (thigh bone). A wedge of bone is resected from the inner side of the thigh bone to realign the patients lower limb and offload the sore lateral compartment of the knee. The surgeon employs Patient Specific Instruments to guarantee precision on the cut and restore the patient's ideal alignment.


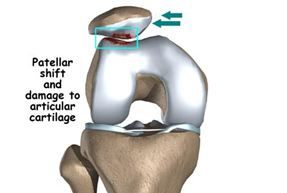
- Tibial Tubercle Osteotomy: This type of osteotomy is less common and is typically performed in conjunction with other knee procedures. It involves cutting and repositioning the bony bump at the top of the shinbone (Tibial Tubercle) to improve patellofemoral alignment and/or offload a sore/arthritic anterior compartment of the knee. The main indications are patella instability/dislocation and anterior knee pain.
High Tibial Osteotomy
What is a High Tibial Osteotomy?
A High Tibial Osteotomy (HTO) is a surgical procedure that involves cutting and repositioning the upper part of the tibia (the shinbone) to relieve pain and improve function in patients with isolated knee osteoarthritis or other conditions that cause malalignment of the knee joint and need to be corrected.
An HTO aims to shift the weight-bearing load away from the damaged part of the knee joint, typically the inner (medial) side, to the healthy side. Doing so reduces the load on the damaged part, and the joint can heal and function more effectively.
Who is Suitable for High Tibial Osteotomy?
High Tibial Osteotomy is commonly indicated for patients with osteoarthritis isolated to a single compartment (unicompartmental osteoarthritis) and too young to consider undergoing Knee Replacement Surgery, usually under 50-55 years old.
The aim is to take pressure off the damaged area and shift it to the other side of your knee with healthy cartilage.
There are also important criteria to be a candidate for an osteotomy around the knee
- Not smoking for six weeks before and six weeks after surgery
- BMI below 35
- Isolated disease
- Young than 55 years old
The most common scenario is a patient with a bowed leg because the knee's inner (medial) part has arthritis and is worn away.
How is HTO Suitability Determined?
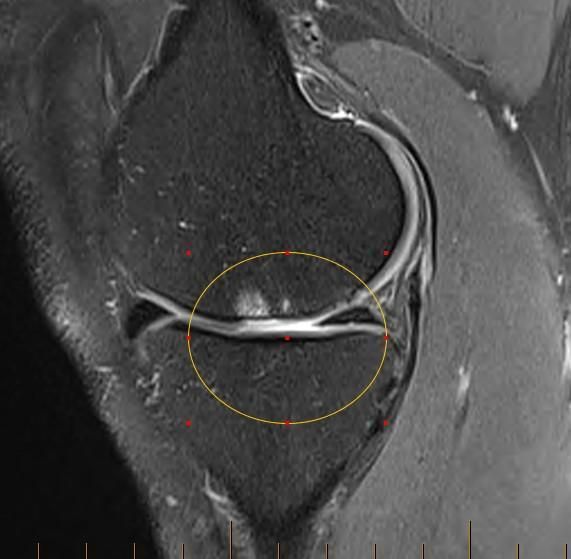
You will require an MRI scan of your knee to investigate suitability for surgery. This ensures other critical parts of your knee are also not damaged by arthritis.

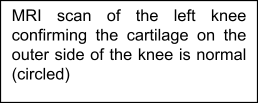
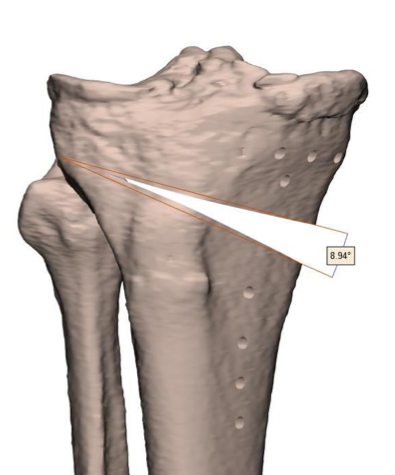
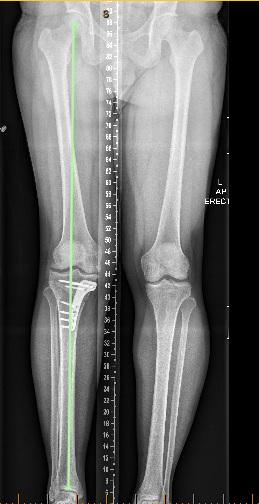
Long X-Ray Required
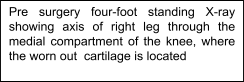
A special long x-ray (Maquet views) is taken while standing from your pelvis to your ankles. This x-ray helps calculate where most of the load is distributed in your knee, the severity of the deformity affecting the knee, and the degree of correction required to unload the diseased part of the knee.

How is High Tibial Osteotomy Performed?
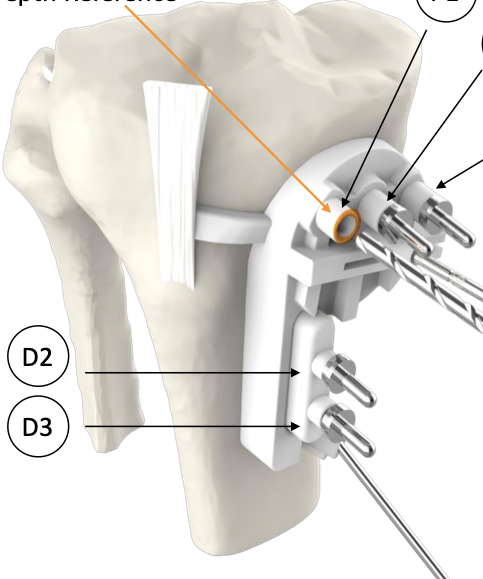
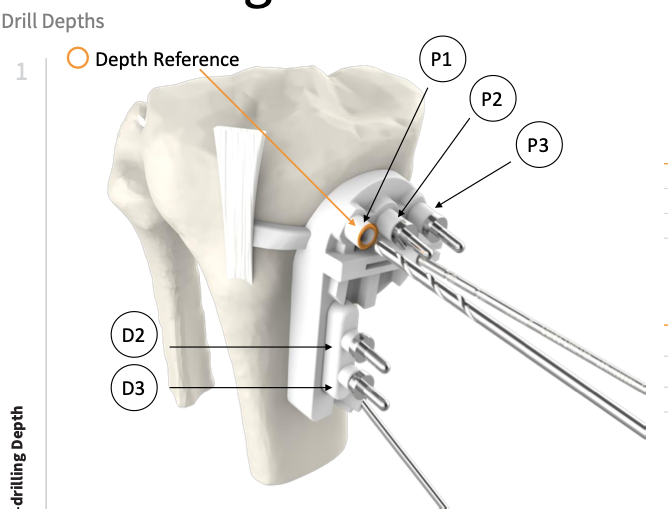
- You will require a general anaesthetic + regional anaesthesia. Your doctor utilises Patient Specific Instrumentation during the surgery to increase the accuracy of the surgery.
- The initial part of the surgery involves inspecting the inside of the knee with the arthroscope.
- Your surgeon plans the amount of correction needed, and Specific 3D oriented instruments and plates will be customised specifically for your case.
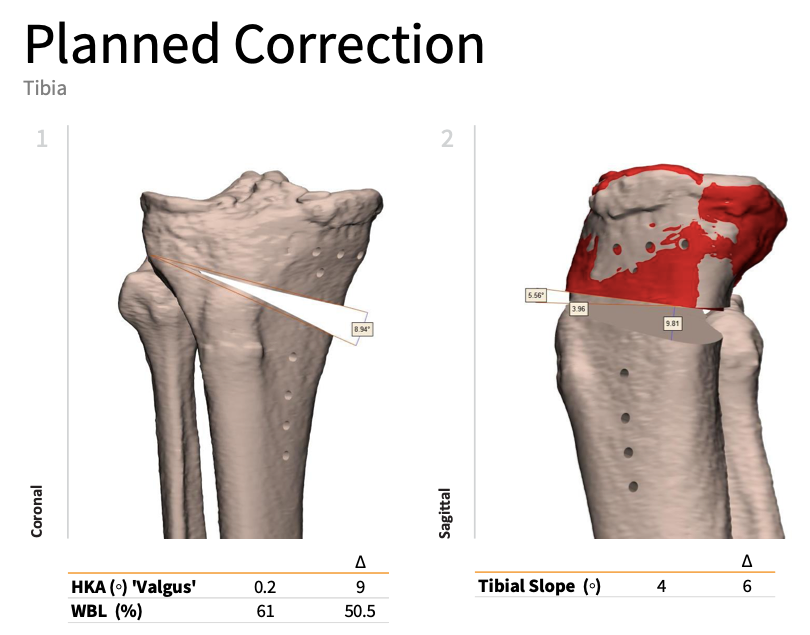
- The PSI jig is attached to your tibia, respecting landmarks, and the plate holes are drilled accordingly.
- Once the PSI jig is secure and the position is confirmed, a Precision-Saw is used to perform the cut.
- With the use of lamina-spreaders and osteotomes, the gap in your bone is creed according to the planned
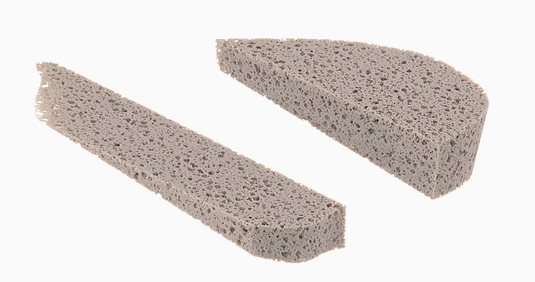
- Custom-made bone allograft wedge-shaped and bone filling are introduced in the gap
- The custom-made plate and screws are then used to hold the osteotomy in position.

- Post-operative x-rays confirm adequate plate and screw fit, accurate correction and bone graft inserted in the medial wedge gap

Recovery After High Tibial Osteotomy
Will I Need To Wear A Brace?
Yes, you will need a brace for six weeks following your surgery. The brace will initially only allow the knee to fully straighten and allow 120 degrees of bend. At six weeks mark and after x-rays confirmation, the brace should be discontinued
Can I Put Weight On My Leg?
You will be allowed to touch weight bearing for the first two weeks. After that, it will progress accordingly
- Weeks 2-4: 25-50% of body weight
- Weeks 4-6: 50-75% of body weight
- Weeks 6-8: 75-100% of body weight
How Long Does It Take To Make A Full Recovery?
The bone will take up to 12 weeks to heal, but the full recovery to restore range of motion, quadriceps strength, balance, and proprioception may take a few more months.
Tibial Tubercle Osteotomy
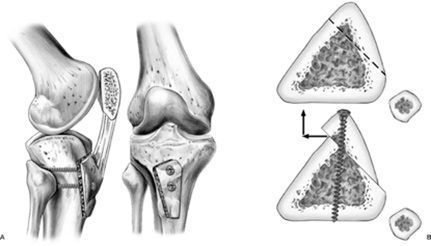
How is the Surgery Performed?
You will be admitted to the hospital on the day of your surgery.
Your surgery will be performed using a general anaesthetic or a spinal anaesthetic, depending on your and your surgeon’s preference.
The initial part of the procedure involves inserting the arthroscope into the knee joint and inspecting the joint for any damage to the articular cartilage surfaces or a potential lateral release if the lateral retinaculum is found too tight.
At this stage, any cartilage injuries can be treated.
A 9-14 cm incision is then made on the front part of the knee. A 6 cm long bony segment of the patellar ligament attachment (called the tibial tubercle) is repositioned and held in position with two screws to heal in this new location.
The TTT is performed to move the attachment to the inner side (medial) or further down the tibia (distal). The surgical incision is usually closed with dissolvable subcuticular sutures.
Frequently Asked Questions
How will my pain be controlled after surgery?
A local anaesthetic around the knee will decrease your pain during surgery. The anaesthetist often injects an additional anaesthetic called a nerve block while you are asleep. This has a significant impact on reducing the amount of pain you experience.
In addition, you will be given long-acting analgesic tablets to reduce your pain. You will be sent home from the hospital with a prescription for oral pain medication. The most commonly prescribed medications include anti-inflammatories (e.g. Celebrex), regular panadol and breakthrough pain medication (e.g. Tapentadol or Endone).
Following week three, you will decrease your pain medication use before physiotherapy and bedtime. Most patients will not require any pain medication past six weeks.
When will I follow up with my surgeon after surgery?
Your first postoperative visit will be with your surgeon in 2 weeks. This appointment is critical for checking your incision healing and range of motion and answering any questions.
You will then follow- up with your surgeon
- six weeks after surgery,
- 12 weeks after surgery,
- 6 months after surgery, and
- one year after surgery.
X-rays will be ordered at each visit until the 3-month mark to ensure the TTT is healing. You will discuss your return to higher-level activity six months post-op with your surgeon. After your first year, you are usually discharged.
Do the screws need to be removed in the future?
Some patients do find irritation from the retained hardware; in these cases, both screws can be removed during a day surgical procedure.
When will I start physiotherapy?
You will start physiotherapy beginning the day after surgery in the hospital, which will continue once you are discharged. You will need to see your physiotherapist generally twice a week for the first six weeks, once a week for the next six weeks, and then reduce the visits from this time.
What will I do during physiotherapy?
The primary goal of physiotherapy is to initially increase ROM so that you do not get stiff following surgery. You will then begin to work on increasing strength and balance after surgery. You will receive a detailed protocol for what you should and should not do during each postoperative phase. You will provide this to your physiotherapist.
When do I need to wear my brace?
You must wear your brace anytime you move around on your crutches. You will use your brace for 6-8 weeks on average.
How long will I need to use my crutches?
Depending on how quickly your bone heals and your surgeon’s preference, you must use your crutches between 6 and 8 weeks on average.
When can I drive?
For patients undergoing right leg surgery, you may not return to driving until you have discontinued using your crutches (approximately six weeks). For patients undergoing left knee surgery that does not drive manual vehicles, you may return to driving between 3 and 6 weeks when you are no longer taking pain medication.
When can I shower?
You may shower following surgery with your knee brace off, but you must be sitting down at all times. You will have a water-proof dressing covering your incision. It is advisable to have someone help you get dry and dressed. The knee brace must then be re-applied.
When can I go back to work?
This will be different for each patient and depends mainly on the type of work you do. Most patients working in a sedentary position or desk work will return to work in 4-6 weeks. Patients in more labour-intensive jobs may be out of work for up to 12 weeks.
When can I resume my regular activity?
Return to normal activity depends highly on each patient’s definition of everyday activity. Non-impact activities such as walking, swimming, bike riding, and elliptical training can all be resumed in 3-4 months. Higher-demand activities such as running and sports cannot be resumed until at least 8-12 months.
Knee Osteotomy Prognosis
In general, knee osteotomy has a high success rate, with many patients experiencing significant pain relief and improved knee function. However, it may not suit everyone, and some patients may require additional surgery or alternative treatments.
Knee Osteotomy Risks
Like any surgical procedure, knee osteotomy carries some risks, including infection, bleeding, nerve damage, blood clots, non-union, delayed union, and post-operative fracture. Other potential risks include failure of the bone to heal correctly, loss of range of motion, and persistent pain or swelling. Your orthopaedic surgeon will discuss these risks with you before the procedure and take steps to minimise the risk of complications.
What if Knee Osteotomy is Delayed?
If knee osteotomy is delayed, the condition causing knee pain may worsen, leading to more significant damage to the knee joint and increased pain and disability. In some cases, delaying knee osteotomy may result in the need for more extensive surgery, such as knee replacement surgery, which is a more invasive and complex procedure.