Posterior Cruciate Ligament Reconstruction
What is a Posterior Cruciate Ligament (PCL)?
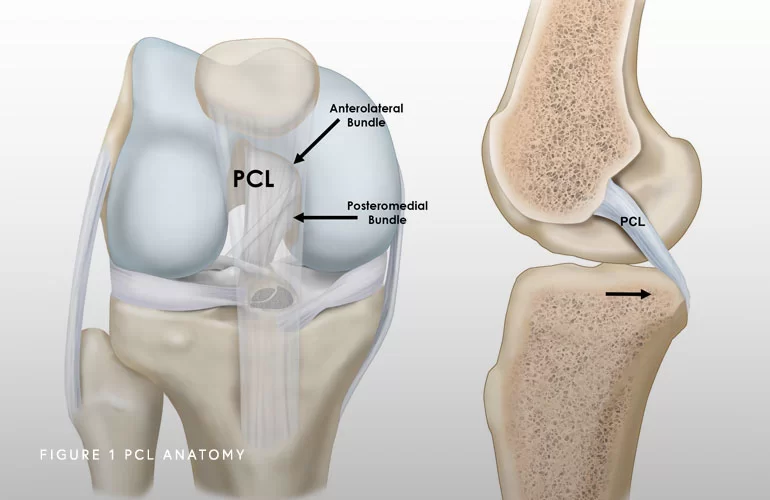
The posterior cruciate ligament (PCL), one of the four major ligaments of the knee, is situated at the back of the knee. It connects the thigh bone (femur) to the shinbone (tibia). The PCL limits the backward motion of the shinbone.
Injury to the PCL is less common than the anterior cruciate ligament (ACL), but it can still cause significant pain and instability in the knee.
What is Posterior Cruciate Ligament Reconstruction?
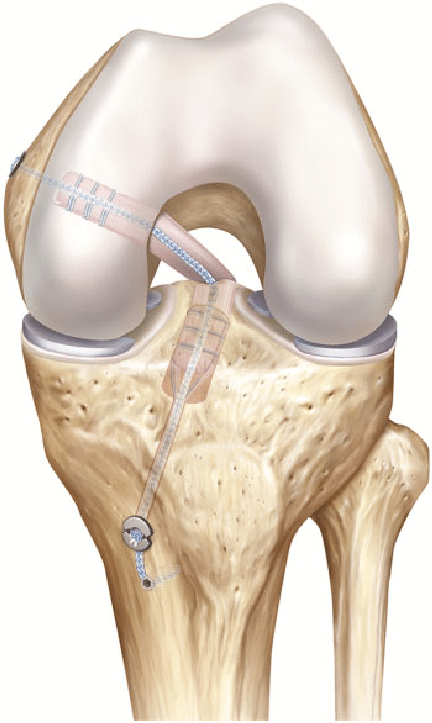
PCL reconstruction is a surgical procedure that involves replacing the damaged PCL with a new ligament graft. The surgery is usually performed arthroscopically, which means that small incisions are made around the knee, and a camera and surgical instruments are inserted to reconstruct the damaged ligament. In a modern way, Adjustable Suspensory Devices are employed to perform an All-Inside Technique through partial length femoral and tunnels where the graft is secured.
Who is Suitable for PCL Reconstruction?
PCL reconstruction is typically recommended for patients who have experienced a complete tear or significant injury to the PCL and have clinical instability for activities of daily life or to practise some contact, pivoting sports. Patients with multiple knee injuries or significant knee instability may also be suitable candidates for the surgery. An orthopaedic surgeon will evaluate the patient's injury, medical history, and overall health to determine if PCL reconstruction is the right option.
What are the Benefits of All-Inside PCL Reconstruction?
PCL reconstruction can provide several benefits for patients, including:
- Increased Knee Stability: The new ligament graft can stabilise the knee joint, allowing patients to engage in physical activities without fear of instability or further injury.
- Improved Knee Function: PCL reconstruction can improve the knee joint's range of motion and overall function.
- Faster Recovery: Arthroscopic PCL reconstruction is a minimally invasive procedure, meaning patients can expect a quicker recovery time than traditional open surgery.
- Graft Preserving: all-inside PCL technique allows the surgeon to preserve tissue without sacrificing graft length and diameter
- Bone Preserving: partial length tunnels preserve cortical bone for unlikely revision surgery in future
What are the Types of Grafts used for PCL Reconstruction?
Two primary types of PCL reconstruction graft are utilised: autograft and allograft.
- Autograft involves using a patient's tissue, typically from the hamstring or quadriceps muscle, to create a new ligament graft.
- Allograft uses tissue from a donor to create a newly reconstructed ligament.
The choice between autograft and allograft reconstruction will depend on the patient's unique circumstances, including the severity of the injury, the patient's age and overall health, autograft availability and the surgeon's preference.
Preparation Before PCL Reconstruction
Preparing for PCL reconstruction surgery involves several steps to ensure the best possible outcome.
- Before surgery, you will typically undergo a medical evaluation to assess your overall health and identify any underlying conditions that may affect the surgery or recovery. Your medical history, medications, and allergies will be reviewed.
- Imaging tests such as X-rays, MRIs, or CT scans may be performed to provide detailed images of the knee joint and help the surgeon plan the procedure.
- You may be asked to stop taking certain medications or supplements in the weeks leading up to the surgery, as these can increase the risk of bleeding or interact with anaesthesia. It's essential to follow the surgeon's instructions carefully regarding medications.
- You will typically be asked to avoid eating or drinking anything for some time before the surgery, as directed by the surgeon or anesthesiologist.
- You should arrange for someone to drive you home after the surgery, as you may be unable to drive yourself. Also, arrange for someone to assist you with cooking, cleaning, and shopping during recovery.
- You should quit smoking for at least six weeks before the surgery, as smoking increases the risk of complications and slows healing.
- You will be referred to a physical therapist before the surgery to help strengthen the muscles around the knee and improve the range of motion. This can help with recovery after the surgery as well. Usually, the same physiotherapist will follow you up after surgery.
Following the surgeon's instructions carefully in the weeks leading to PCL reconstruction surgery is essential to ensure the best possible outcome.
PCL Reconstruction Procedure
Surgery involves the reconstruction of the torn ligament using a tissue graft taken from another part of the body or a donor.
Surgery is usually carried out with the assistance of an arthroscope, using a few small incisions. The basic steps involved in PCL reconstruction are as follows:
- The surgeon inspects the knee and removes any remains of the native PCL using an arthroscopic shaver. Care is taken to preserve the ligament of Wrisberg if it is intact.
- The donor's tendon is harvested from the quadriceps tendon or hamstring tendon.
- The soft tissue around the femur is debrided to assist the graft insertion.
- A tunnel is created in the femur at the anatomic attachment site of the anterolateral bundle at the anteromedial wall of the intercondylar notch. This tunnel is drilled about 8 mm from the articular surface of the medial femoral condyle.
- The tibial attachment site is also prepared by identifying the normal attachment of the PCL at the bottom of the PCL facet.
- For placing the graft, a tibial tunnel is created for the anatomic insertion of the PCL on the tibia.
- Once the tunnels are drilled, the sharp edges and soft tissues around the exit site of the tunnel are smoothed with a rasp.
- The tendon allograft is inserted in the femoral tunnel and fixed with an adjustable suspensory fixation device.
- The graft is then pulled through the tibial tunnel and secured by an ASF device.
- The graft is made taut distally by removing any slack in the graft.
- After fixation, normal posterior stability of the knee is assessed by employing the posterior drawer test.
- The incision is closed with sutures and covered with sterile dressings.
After PCL Reconstruction
You will be monitored in the recovery room and may need to stay in the hospital overnight. Pain medications and physical therapy will be prescribed to manage pain and aid recovery. You will need to wear a knee brace for several weeks after the surgery and may need to use crutches for support.
Postoperative Care following PCL Reconstruction
Postoperative care following the surgery is crucial to ensure proper healing and successful recovery. Here are some general guidelines for postoperative care:
Pain management
You will likely experience pain and swelling after the surgery. The surgeon will prescribe pain medications and may recommend ice packs or compression wraps to help manage pain and reduce swelling.
Immobilisation
The knee may be immobilised with a brace or splint for several weeks after surgery to protect the reconstructed ligament and promote healing. The surgeon will provide instructions on when and how to use the brace. Ideally, an Off-Load PCL brace is recommended. See the link
https://www.ossur.com/en-au/bracing-and-supports/knee/rebound-pcl

Weight-bearing and mobility
You may be restricted from full weight bearing on the affected leg for some time after surgery, depending on the extent of the injury and the type of reconstruction performed. Physical therapy may be prescribed to help regain strength, mobility, and range of motion in the knee joint.
Wound care
You should keep the surgical incision clean and dry to prevent infection. The surgeon will provide instructions on caring for the incision and when to remove the stitches.
Follow-up appointments
You will have several follow-up appointments with your surgeon to monitor your healing progress and adjust the treatment plan.
Activity modification
You should avoid activities that stress the knee joint, such as running or jumping, for several months after surgery. The surgeon may advise when it is safe to return to normal activities. The brace should be continued for eight weeks, and only closed-chain exercises are allowed in the first 12 weeks. See more details in rehabilitation protocols in useful links.
Smoking cessation
You should abstain from smoking six weeks before and after surgery, as smoking slows healing and increases the risk of complications.
Following your surgeon's instructions carefully during the postoperative period is essential to ensure the best possible outcome. Any concerns or questions should be discussed with the healthcare team.
Risks and Complications of PCL Reconstruction
Knee stiffness and residual instability are the most common complications associated with PCL reconstruction. The other possible complications include:
- Numbness
- Infection
- Blood clots (Deep vein thrombosis)
- Nerve and blood vessel damage
- Failure of the graft
- Loosening of the graft
- Decreased range of motion
What if PCL Reconstruction is Delayed?
Delaying PCL reconstruction can lead to further knee instability, cartilage damage, and a potentially higher risk of developing knee osteoarthritis. It's essential to seek medical attention as soon as possible after a PCL injury to prevent further damage and ensure the best possible outcome.